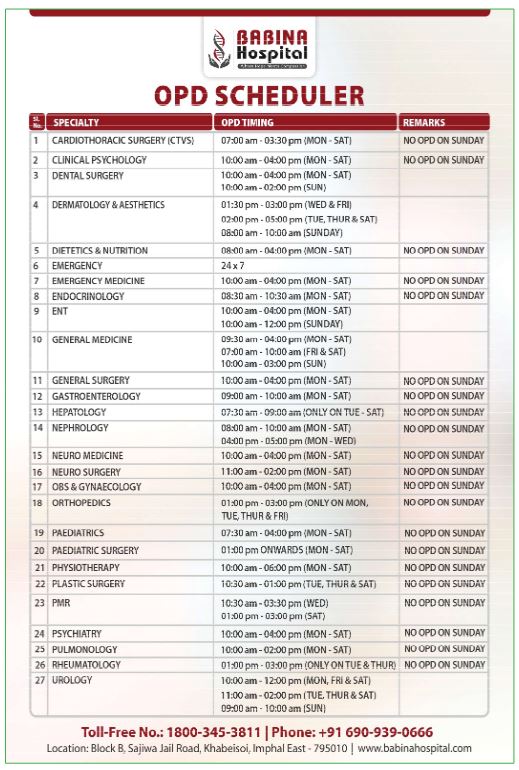
By Nicholas Hunt and Jarryd Daymond, University of Sydney in Sydney
A new way of delivering oral insulin could sidestep some of the challenges people living with diabetes encounter when injecting insulin.
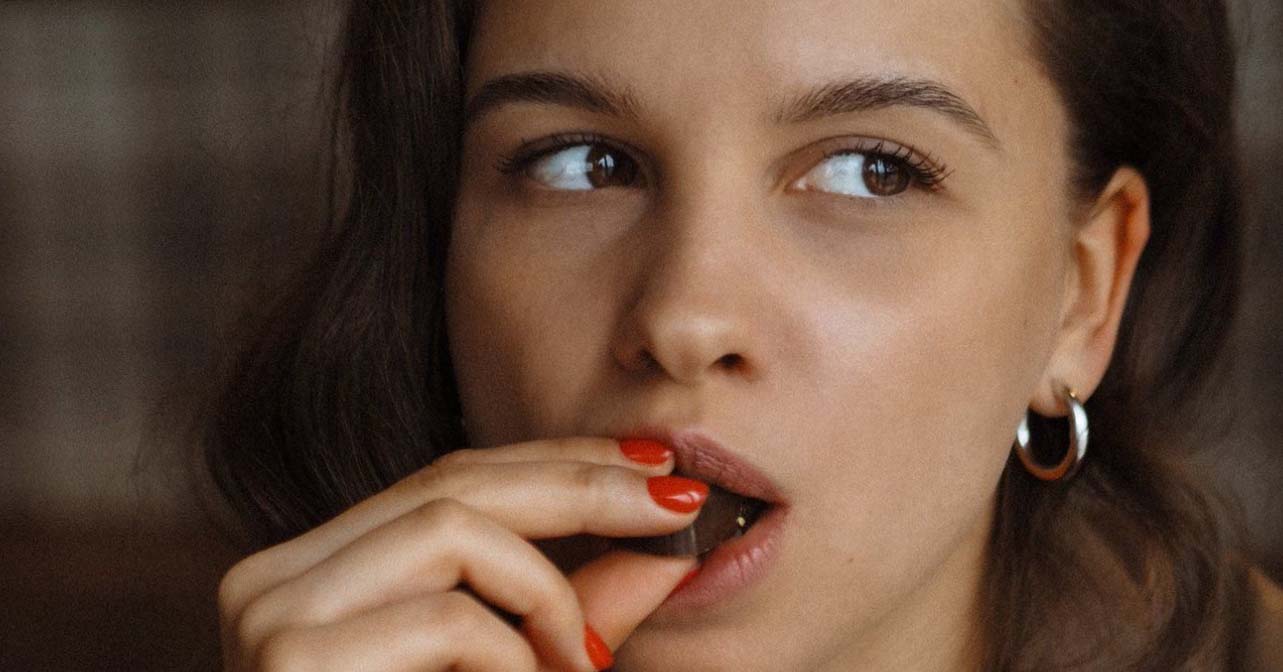
People with diabetes may soon be able to replace injections with more palatable oral forms of insulin, such as sugar-free chocolate, thanks to advances in nanotechnology.
Insulin injections are a daily reality for many of the 150 to 200 million people globally who need insulin. Everyone with type 1 diabetes needs insulin, and 20 to 30 percent of people with type 2 diabetes will also need it over the course of living with the condition.
These injections, although essential for ensuring people living with diabetes have enough insulin in their bodies to make sure their blood sugar levels don’t spike, are not without their own challenges.
Insulin injections can lead to people experiencing low blood sugar or hypoglycemia because they may have injected more insulin than their body needs or not timed their injections correctly around meals. Other side effects include weight gain and needle phobia.
Such challenges especially affect young patients, the elderly and those with cognitive or physical impairments.
Historically, taking insulin orally instead of injecting it has been ineffective, primarily due to such treatments being destroyed by acid in the stomach or being poorly absorbed by the gut.
But new research has introduced a way of delivering oral insulin that sidesteps these problems through the use of nanotechnology.
The system encapsulates the insulin inside nano-sized carriers known as quantum dots, which are roughly 1/10,000th the width of a human hair, or a millionth the size of your finger. These nano-carriers protect the insulin from being degraded as it moves through the stomach and are more easily absorbed in the small intestine.
The carriers are then able to release the insulin at sites in the body where it is most needed.
The point at which the insulin is released is influenced by the body’s blood sugar levels and the presence of enzymes, small proteins that break down sugars in the blood.
How this process works is that the insulin is encapsulated inside a coating that reacts with its environment. The coating is broken down by enzymes released when there are high concentrations of sugars in the blood.
When blood sugar is high, there is a rapid release of insulin, and importantly when it is low, insulin is not released.
This is a more practical and patient-friendly method of managing diabetes, because it greatly reduces the risk of a low blood sugar event, as the insulin is released in a more controlled way, unlike injections in which it is released in one hit.
Following the completion of pre-clinical studies, the next steps towards bringing this technology to patients are to ensure its efficacy and safety through human trials, understand any potential side effects, and address how the nano-carriers can best be produced and distributed at scale.
Human trials are expected to start in 2025.
The rising prevalence of diabetes in the Indo-Pacific region is a significant health challenge.
It affected an estimated 296 million adults in 2021 and is projected to increase to 412 million by 2045.
Type 2 diabetes, often associated with lifestyle and environmental factors, contributes to major health complications like heart disease, stroke, blindness and kidney failure. These complications lead to increased mortality rates among diabetic patients.
Additionally, the high costs of diabetes care highlight the disparities in access to treatment, disproportionately affecting individuals in lower-income countries and remote areas.
For example, a 10-year-old diagnosed with type 1 diabetes in 2021 could expect to live on average for another 65 years in a high-income country, but only another 13 years in a low-income country.
The introduction of this new method for delivering insulin orally could provide several other benefits for people living with diabetes who are insulin-dependent and inject rather than use an insulin pump.
It may improve the quality of life for patients by reducing the discomfort and stigma associated with insulin injections.
For example, some people can feel uncomfortable injecting insulin because of needles being associated with illicit drug use. Or if they’re experiencing a low blood sugar event, they may feel socially stigmatised if their symptoms are mistaken for intoxication or mental illness.
This method also allows insulin to be stored at room temperature rather than having to be refrigerated. The nano-carrier preserves the protein structure of the insulin and protects it from the environment.
This could extend its accessibility to patients in remote regions and lower-income countries, providing them more effective diabetes treatment and reduced costs related to diabetic complications.
There is also scope for this delivery system to be used to orally administer other injectable diabetes medications, for example GLP-1 receptor agonists like Ozempic.
The next generation of the nano-carrier is being developed to treat the causes of type 1 diabetes and other autoimmune conditions.
With the increasing number of people affected by diabetes, the development of new management strategies is critical.
If successful, this technology could offer a significant change in how diabetes is treated with the potential to simplify diabetes management for millions of people, particularly benefiting those who face barriers to traditional insulin therapy.
Dr Nicholas Hunt is a senior lecturer in the School of Medical Science at the University of Sydney and leader at the Biogerontology laboratory at the ANZAC Research Institute. His research interests centre around the development of new nanomaterials for use and translation in clinical medicine. He has worked on the development of quantum dots and organic nanoparticles for biological applications including the transportation of pharmaceutical agents, biologics, RNA and gene therapy.
Dr Hunt is co-founder and CEO of Endo Axiom, which will be taking these therapeutics to clinical trials.
Dr Hunt’s research has been supported by the Australian Diabetes Society, the University of Sydney, the Sydney Medical School Foundation, the National Health and Medical Research Council (NHMRC), the Medical Research Future Fund (MRFF), Therapeutic Innovation Australia and the Caenorhabditis Genetics Centre.
Dr Jarryd Daymond is a lecturer in strategy, innovation and entrepreneurship for the University of Sydney Business School and a Sydney Nano Institute Early Career Researcher Ambassador. He studies the processes and practices of responsible innovation of emerging technologies, including the responsible innovation of digital, quantum, and nanotherapeutic technologies. Dr Daymond is involved in projects to commercialise oral insulin and develop online cognitive-communication treatment platforms.
Originally published under Creative Commons by 360info™.