As stranded Manipuris continue to pour back home by land and air routes, Coronavirus positive cases continue to climb in the state. At this point, probably about half of the approximate 50,000 who had registered with the Government of Manipur helpline, Tengbang, indicating they want to return, are back and the number of positive cases has just crossed the 150 mark, and of them a about 100 are still active and therefore not discharged yet from the hospitals where they have been kept in isolation. It is therefore with an understandable measure of alarm that continued inflow of stranded people is viewed generally. This is particularly so as most Indian metropolises are today fast developing into hot zones of the virus, with possible community transmission already underway in some, and hence this upward trend in the rate of virus infection amongst later returnees. A rough estimate arrived at through extrapolation from this trend should be about 300 positive cases, or at worst 500 positive cases for Manipur to handle by the time all of the 50,000 who want to return are back in their home state in say another one month. This is if the state is successful in not allowing the virus to spread into the community by an effective regime of tests and quarantine of all returnees. If there have been some fringe cases of community transmission, as it does seem from the report of a nurse in Churachandpur who got the virus without any travel history, the response must be to also contact trace and quarantine them as well. If community spread is successfully contained, then from the projected 300-500 positive cases, probably 200 to 300 would already have recovered, leaving the state with 100 to 200 active cases to deal with after the current rush of returnees is over.
Amidst all the anxieties, certain other important data tend to be overlooked. The most important of these are: One there have been no fatalities. If the national average is to be adapted for calculation, at least four should have died from the 150 or so tested positive so far. Two, not only has there been no fatalities so far, there have also been no acute COVID cases needing ICU and ventilator life support. In other words, all those who tested positive were either asymptomatic or else mildly symptomatic only. Why has this been so will be for scientists working in BSL-4 laboratories all over the world now, racing to size up the virus and find a vaccine or drug for a comprehensive solution to the devastation it is causing, to answer for us. However, in all probability this answer will not be forthcoming for several months, if at all. Speculations in the scientific community are, the virus is constantly mutating, and as it hijacks human cells and multiplies itself, it is by error copying some genetic materials of the host cells into its own replicas. If this speculation is true, it could be the virus is losing some of its pathogenetic qualities, and thankfully for us all. We do hope something of this is happening. The other reason could be, generally those who go out of the state, either as students or else as job seekers, are young and healthy, therefore have strong immune systems to ward off the ill effects of the virus. We have however also seen one not so young cancer patient who tested positive completely recovered. Whatever the case may be, the truth is, we have seen no COVID fatalities so far, and we do hope we will not see any ever.
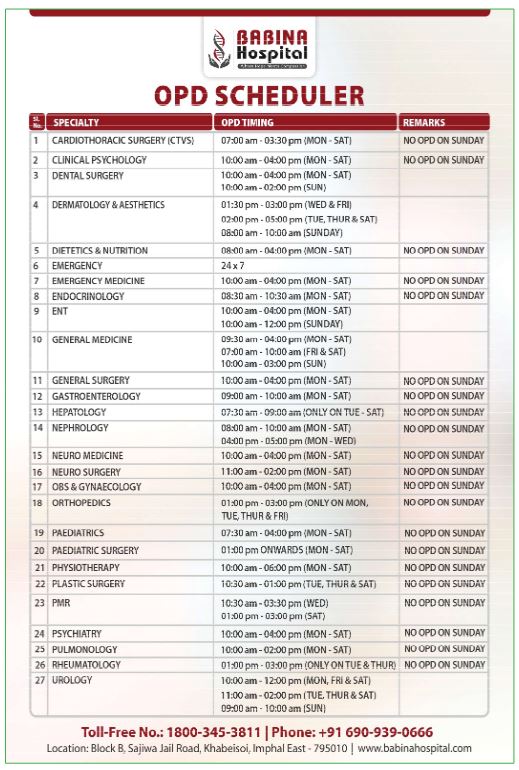
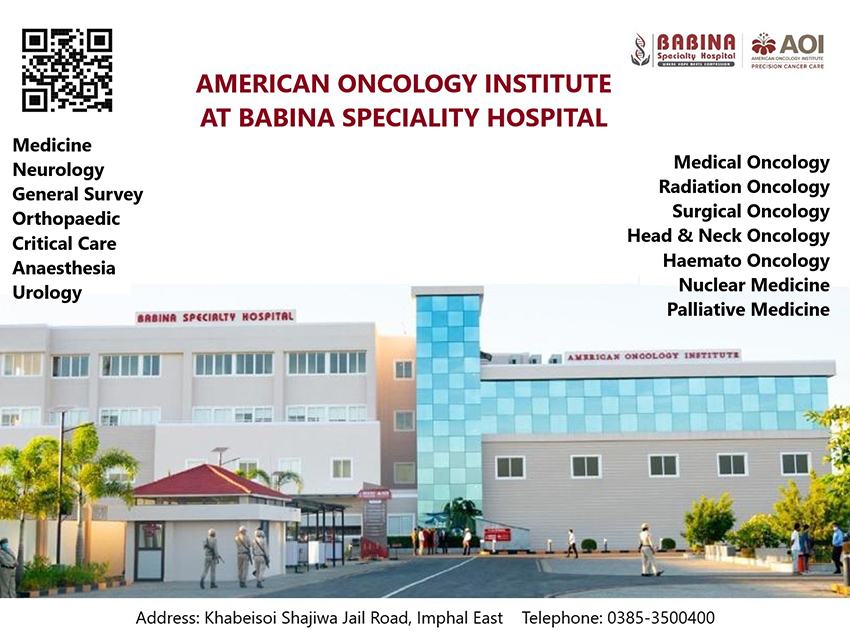
With this picture in mind, the other important question to be tackled is, if in the event of 500 or more turning positive of the contagion, and the state is left to deal with 300 or so active cases at any time, would its existing health infrastructure be adequate to live up to this challenge? To use a term now made popular, can we still keep the state’s pandemic spread curve flat so that our health infrastructure is not overwhelmed? Reports are, already health workers are under pressure because of manpower shortage. Several recommendations have been forwarded from different quarters. Among these is the idea of setting up of a COVID exclusive hospital. As an emergency measure, this may be a little too ambitious, but this should make for sound long-term measure to meet recurrences of COVID outbreaks, which scientists think is very much a possibility, as well as to tackle other communicable deadly diseases of the future, which again scientists are of the opinion is a reality considering among others the radical changes in world climate. Perhaps it would also be a good idea to give such a hospital a more generic name covering all communicable diseases, and not narrow its focus to just one. There has been one more suggestion in the regard, one which takes into consideration a general misconception, including seemingly by policy makers – that is, there is a distinction to be made between coronavirus and COVID as the WHO pointed out on February 11. The former is a dangerous virus and the latter is the disease this virus causes in humans. The fact also is, on the average 80 percent of people who contracts the virus do not become ill with COVID. Again, of the 20 percent who become ill, only around 10 percent become severely ill to need life support system intervention. In the case of Manipur, as we are witnessing today, only very few who have tested positive of the virus have shown symptoms of COVID and of the few who did have mild symptoms, none have needed ventilator support. This being what it is, instead of hospitalising every person who have tested positive of the virus, only those with symptoms can be taken to the hospitals. The asymptomatic and mildly symptomatic cases can then be kept in special quarantine facilities near the hospitals while they recuperate under supervision of some health workers. In case any of them begin to show symptoms, they can be transferred to a hospital. This way, our health infrastructure will not be put under undue duress.