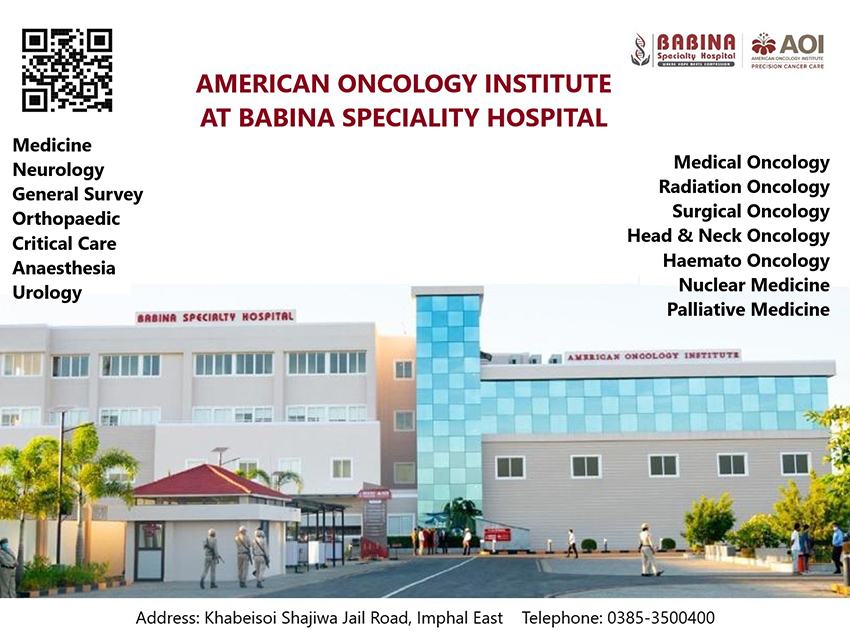
The COVID lockdown has finally been lifted even as it was midway in the sixth month, and except in the containment zones where restrictions still continue, normal life is supposed to be ushered back in. However, the state government has failed to prepare a comprehensive policy and Standard Operating Procedures (SOPs) for the hospitals to provide healthcare to both the Covid and Non-COVID Patients of Manipur.
This is as per an order of the Ministry of Home Affairs on August 29. However, the two biggest public hospitals of Manipur are still not accepting non-COVID patients claiming a shortage in capacity to handle the additional responsibility.
There have been cases of fatalities, which included a pregnant woman, due to the denial of medical care to the patients since the closure of OPDs and wards of the two public hospitals, the Regional Institute of Medical Sciences (RIMS) and Jawaharlal Nehru Institute of Medical Sciences (JNIMS).
Now, everyone knows that lockdown is to flatten the curve of COVID-19 pandemic. Flattening the curve is meant to reduce the number of cases at any given time by inhibiting new infections and allows healthcare services to better manage the volume of patients. Moreover, lockdown is to prepare all fronts to fight the COVID-19 pandemic successfully.
Amidst the COVID-19 pandemic, many Non-COVID-19 patients have also died for want of proper healthcare service. Many patients cannot reach hospitals and clinics, and cannot consult doctors even privately due to the lack of clear guidelines or SOPs for Non-COVID patients.
A lot has been said and discussed in reports here about the need for the hospitals to be prepared fully for Non-COVID patients and how to tackle spread of COVID-19. But what is found missing at the moment is a proper policy and programme or SOPs at the hospitals for both the Covid and Non-COVID patients.
Meanwhile, sources say that many doctors and health care workers of the public hospitals are reluctant to see patients whose COVID-19 status is not confirmed. Moreover, there are no mandatory tests for COVID-19 for every patient before consultation with doctors at these public hospitals.
Here the questions that crop up are – why should doctors and health care workers run away from their professional risks and challenges? Should soldiers take leave when war breaks out? Why should hospital doors be shut down to the Non-Covid patients when we have to learn to live with Covid-19?
Amidst the lockdown, the OPDs of the RIMS were functioning for some time taking patients who had already registered through their mobile phones prior to coming to the hospital, before the surge of COVID-19 spread amongst the doctors and health care workers of the hospital in the month of July.
To a query on when the OPDs of RIMS might reopen and treat Non-COVID patients, RIMS Medical Superintendent Dr. Ch Arunkumar told FPSJ Review on September 4 that the RIMS is not ready to accept Non-COVID patients by opening OPDs and taking in-ward patients as of now.
However, the Casualty and Emergency block is open 24×7 and they are taking care of about 150 to 200 patients a day. Even patients who are not emergency in nature visit Casualty and Emergency Ward, added Dr. Arunkumar.
On a further query Dr. Arunkumar said, there is no possibility of opening OPDs until and unless the upswing of the COVID-19 positives cases come to a down swing or a decision to open is taken, whichever is earlier. The OPDs were closed down since 66 doctors and health care workers of the RIMS tested COVID-19 positive. At the moment also four health care workers of the Casualty and Emergency Ward have tested COVID-19 positive.
Meanwhile, the Chief Secretary of Manipur Government has asked for an increase in the capacity of COVID Ward from 78 to 300. “If we are compelled to increase the capacity to 300, the chances of opening OPDs in the very near future is dim as maximum number of doctors, nurses and other health care workers have to be engaged and more structures are needed for their quarantine,” Dr. Arunkumar added.
Moreover, Medical Superintendent of JNIMS, Dr. T Rajen told FPSJ Review on September 4 that the JNIMS is not ready to open OPDs and other wards for Non-COVID patients as of now. But casualty and emergency patients are taken care of.
Notably, in district hospitals also mostly casualty and emergency patients are being treated during this lockdown.
Chief Medical Officer of Bishnupur district, Dr. Laishram Gojendra told FPSJ Review that emergency patients irrespective of COVID-19 positive or Non-COVID are given treatment. However, in-ward patients cannot be taken due to the lack of doctors, nurses and other health care workers besides infrastructure.
On the other hand, Chief Medical Officer of Jiribam district Dr. Elangbam Oken told FPSJ Review that Non-COVID patients including those not emergency in nature are given treatment at the Casualty and Emergency Ward of Jiribam District Hospital, at Ningshing Khul. Ten beds for patients who need further stay in the hospital are also kept ready as a general ward. For Jiribam district COVID-19 positives are given supportive treatments at the Covid Care Centre opened at Harinagar, added Dr. Elangbam Oken.
Regarding non-opening of OPDs at the RIMS and JNIMS, it is pertinent to ask a few questions. Is it due to the overwhelming of the hospitals with COVID-19 patients that all resources are directed towards it and not many are left for the Non-COVID patients? Is it due to the lack of professional commitment and determination? Is it simply due to the negligence of the Non-COVID patients by the state government?
However, public health and community medicine experts suggest that continuous health care can be given to both the COVID-19 and Non-COVID patients by reorienting the existing hospital or health care set-up, human resources and testing.
Regarding hospital set-up, the entry point for Casualty and OPD should be only one while tele-consultation and appointment system as far as possible for non-emergency cases should be encouraged. Triaging patients at entry point with screening – emergency, symptomatic, cold cases etc. Next level can have three or four parallel stations to tackle various conditions. The next level can have at least two stations for handling conditions needing senior doctors’ consultation. Manpower from all departments should be posted at the entry levels. Rapid antigen testing facilities for emergency cases should be given. OPD cases apart from ILI/SARI should be decided by the Hospital Covid Committee.
Experts further suggest separate wards to keep suspects for all patients. Better to have another separate ward for COVID-19 positive patients who will be requiring treatment that cannot be done at the usual Covid Care Centres or District Community Health Centres. Dedicated Operation Theatre, dialysis machine and other diagnostic equipment like USG, X-ray machine, ECG, etc. in separate blocks should be arranged.
For Infection Prevention and Control (IPC), the current SOPs should be followed and the buddy system should be adopted. In each category leaders should be identified to monitor and hand hold IPC practices. There should be adequate supply of PPE with rational use – need to devise their own rationale for use of PPE.
Entry of the patient party or attendant should be restricted to two and frequent rotation of the patient party/attendant should not be allowed. One attendant should be allowed for 5 to 7 days followed by self-isolation at home for another 7 days by informing the District Surveillance Officers (DSOs).
Human resource is key in running hospitals to ensure continuous health care to both COVID and Non-COVID patients. Experts further suggest department-wise pooling of junior doctors, senior residents and junior residents from all departments. Covid duty roster system can be adopted and rationalised to facilitate continuous supply, smooth functioning, and periodic testing. Continuous duty roster for five days followed by seven day’s quarantine for health care staff. Quarantine facilities for Health Care Workers should be increased. Minimal staff in one shift will be needed as the number of patients is less.
Testing of Hospital Staff for antibody – risk stratification of the health staff of all categories – doctors, can be done at the last. Testing for Antigen – regular testing at the end of seven days’ quarantine after duty for all staff, should be done. Normally, no immediate testing will be required after an exposure during the duty days.
If resources are available, testing can be done for all patients. If resources are not sufficient, case to case basis can be done.
Patients are patients, COVID or Non-COVID. Hospitals should be prepared to ensure continuous health care to both COVID and Non-COVID patients and it is not impossible if committed and determined by the State, one public health expert asserted.