By Brian D. Earp, University of Oxford in Chicago
Laws on genital mutilation, gender affirmation and cosmetic genital surgery are at odds, even though they have many similarities.
In Ohio, USA, lawmakers are currently considering the Save Adolescents from Experimentation (SAFE) Act that would ban hormones or surgeries for minors who identify as transgender or non-binary. In April this year, Alabama passed similar legislation.
Alleging anti-trans prejudice, opponents of such legislation say these bans will stop trans youth from accessing necessary healthcare, citing guidance from the American Psychiatric Association, the American Medical Association and the American Academy of Pediatrics.
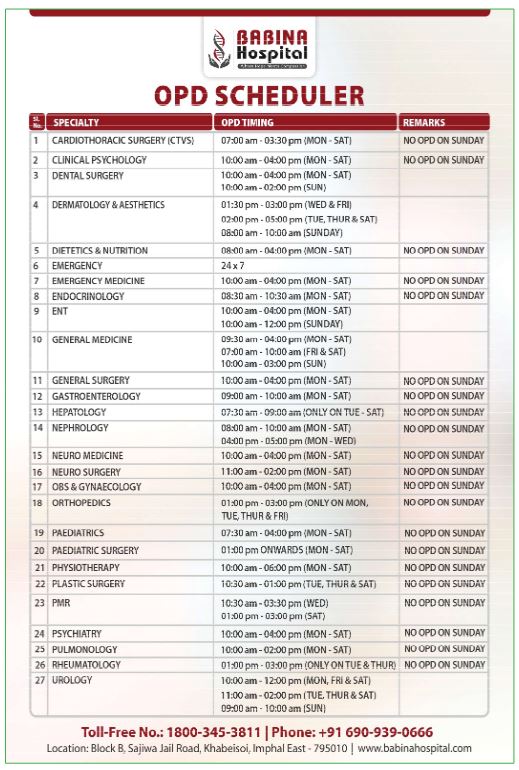
Providers of gender-affirming services point out that puberty-suppressing medications and hormone therapies are considered standard-of-care for trans adolescents who qualify. Neither is administered before puberty, with younger children receiving psychosocial support only. Meanwhile genital surgeries for gender affirmation are rarely performed before age 18.
Nevertheless, proponents of the new laws say they are needed to protect vulnerable minors from understudied medical risks and potentially lifelong bodily harms. Proponents note that irreversible mastectomies are increasingly performed before the age of legal majority.
Republican legislators in several states argue that if a child’s breasts or genitalia are ‘healthy’, there is no medical or ethical justification to use hormones or surgeries to alter those parts of the body.
However, while trans adolescents struggle to access voluntary services and rarely undergo genital surgeries prior to adulthood, non-trans-identifying children in the United States and elsewhere are routinely subjected to medically unnecessary surgeries affecting their healthy sexual anatomy — without opposition from conservative lawmakers.
One group affected by these non-voluntary surgeries are infants born with intersex traits due to one or more ‘differences of sex development’. These traits are often harmless, naturally-occurring variations in human sexual and reproductive anatomy that occur in an estimated 0.018 percent to 0.08 percent of all live births.
Doctors will often recommend risky, even radical surgeries for intersex infants with genital features that differ from cultural ideals of ‘normal’ or ‘typical’. These surgeries attempt to make the child’s body fit within a stereotyped gender binary. They are not to promote the infant’s physical health — which may be impaired by the surgeries.
Studies published between 1955 and 2000 (mostly looking at populations in developed economies) estimate that these surgeries are performed on around one in every 1,000 children, although exact rates are unknown.
Since most intersex surgeries are medically avoidable, are performed without the consent of the affected child, and involve damaging or removing healthy genital tissues, human rights scholar Melinda Jones has called them a “Western form of female genital mutilation”.
The term ‘female genital mutilation’ (FGM) is primarily used to describe (and condemn) non-Western, mostly African, practices. Currently, the World Health Organization (WHO) defines such mutilation as any cutting or alteration of female-typical genitalia that is not done for “medical reasons”.
The WHO’s sex-specific definition includes highly invasive procedures, like excision of the external clitoris and infibulation. But it also counts as FGM relatively minor interventions, such as ‘ritual nicking’ of the clitoral foreskin or hood.
This form of cutting is practiced, alongside male circumcision, by some Islamic sects such as the Dawoodi Bohra.
In 2017, a member of the Bohra community — Dr Jumana Nagarwala — was arrested in Detroit, Michigan on charges of FGM. She was brought to trial for allegedly performing a ritual nick or similar procedure on several young girls.
The federal judge in charge of the case struck down the US anti-FGM law as unconstitutional. However a replacement law was signed by President Trump near the end of his term. The STOP FGM Act of 2020 clarifies that ritual nicking without tissue removal — even for explicitly religious purposes — is now banned as female genital ‘mutilation’.
But like the WHO definition, this law excludes children with intersex traits who undergo medically unnecessary genital cutting, even if categorised by doctors as female at birth.
The language of mutilation is not applied consistently.
Scholars of genital cutting also question why cosmetic labiaplasty surgeries are not condemned as mutilation despite fitting the WHO definition, and despite new findings showing that nearly 20 percent of these surgeries in the United States, between 2016 and 2019, were carried out on under-18-year-old girls.
Few labiaplasties prior to adulthood are done on grounds of physical health. Most are performed to relieve psychological distress in girls who regard their own healthy anatomy as falling outside restrictive gender norms for female genital appearance.
Genital surgeries are also regularly carried out on children who are categorised as male at birth, based on the visual appearance of a penis.
Some of these children have a condition known as hypospadias, where the urethra opening — the hole for urine and semen — is not at the tip of the penis, but is somewhere closer to the body on the underside of the shaft.
Surgical attempts to relocate the urethra opening to the tip remain standard practice, despite a high rate of serious complications, including fistulas, long-term scarring and other damage.
These childhood genital surgeries are rarely needed for physical health reasons. More often, they are motivated by psychosocial concerns, with parents and doctors believing a boy should be able to ‘pee standing up’, or that a child will want his sexual organ to look ‘typical’ for his anticipated gender — even at the risk of losing sexual sensation.
But there is no evidence that non-voluntary surgeries for hypospadias tend to improve psychosocial well-being compared to voluntary surgeries or no surgery.
In addition to children with hypospadias, states now advocating bans on gender-affirming healthcare for trans adolescents allow medically unnecessary genital surgeries on another group of young males without their consent.
This group includes children who have no known differences of sex development nor any medical problems affecting their genitals. The surgery — which occurs over one million times a year in US hospitals — is almost always done for primarily cultural, not strictly medical reasons.
It is circumcision, or cutting and removing the penile foreskin.
The foreskin is often dismissed in US culture as insignificant. However it makes up about 30 percent of the skin system of the human penis. Similar to the female labia and clitoral hood, it is an elastic erogenous tissue that covers and protects the rest of the organ, unless it is removed. Studies suggest it is the most sensitive part of the penis to light touch.
While some American doctors claim that newborn circumcision carries health benefits such as reducing the risk of urinary tract infection (UTI), European doctors dispute these benefits, arguing there’s no medical justification for non-consensual genital surgery on healthy minors.
These doctors stress that circumcision in early childhood, when the organ is not fully developed, carries non-trivial risk. Recent data from California show that 1 in every 100 newborn circumcisions results in late-occurring complications, most of which require surgical repair.
Increasingly, scholars and advocates criticise what they see as biased or selective expressions of concern for children’s bodily integrity. Why is labiaplasty allowed on young teen girls, but not less-severe Islamic ritual nicking — with only the latter defined as ‘FGM’? Why is medically unncessary genital surgery on intersex infants — and non-intersex boys — permitted, while voluntary puberty suppression for trans adolescents with gender dysphoria banned?
Some critics suggest the real motive behind the recent bans is not principled ethics, but conservative policing of the sex/gender binary.
Gender-affirming procedures are considered suspect, because they alter a person’s body to align with a gender category other than the one assigned at birth. Males are expected to identify as boys/men, and females as girls/women. Any other relationship between sex and gender violates traditional norms.
By contrast, even genital operations that are not medically necessary are approved by conservatives if they preserve the status quo of what is considered ‘normal’ for boys and girls.
This includes removing signs of sexual ambiguity in children with intersex traits, reshaping girls’ vulvas through labiaplasty — to make them more ‘feminine’ and petite, banning ‘foreign’ practices like ritual nicking, and altering boys’ penises with hypospadias surgery or circumcision to match cultural norms.
Scholars who study the ethics of genital cutting are increasingly of the view that the same moral and legal principles should apply in this area, regardless of sex or gender.
They argue the key is consent.
For children who are too young to consent, if a genital surgery is not necessary to preserve the child’s physical health, they suggest it should not be performed. Doctors, they argue, should not agree to elective labiaplasties, ritual nicking, ‘normalising’ surgeries for hypospadias or intersex traits, or penile circumcisions in non-consenting minors.
For older teens and adolescents, who have relatively more autonomous decision-making capacity, it is possible that some can give their own valid consent to certain body alterations, such as circumcision — or to medically approved hormone therapies for gender dysphoria, preferably with parental support.
Gender-affirming surgeries for trans minors are not recommended, although in rare individual cases they could be deemed medically necessary prior to age 18. Either way, it is acknowledged that better research on long-term risks and benefits is sorely needed.
And for legal adults, these ethicists claim, there should be the widest leeway for undergoing genital modifications under conditions of informed consent, up to and including purely ‘cosmetic’ procedures with no medical indication.
Brian D. Earp is a senior research fellow in the Uehiro Centre for Practical Ethics at the University of Oxford and associate director of the Yale-Hastings Program for Ethics and Health Policy at Yale University and The Hastings Center. He is a signatory to the 2019 Brussels Collaboration on Bodily Integrity international scholarly consensus statement on the ethics of child genital modification.
Originally published under Creative Commons by 360info™.