By Sangeeta Tanna and Rachel Armitage, De Montfort University in Leicester
COVID-19 has shown that regulatory processes can fail anywhere, allowing poor-quality medicines through. A new detection test could help shield consumers.
It’s the lesser-known pandemic: poor-quality medicines cause alarming rates of death and worsened illness across the globe.
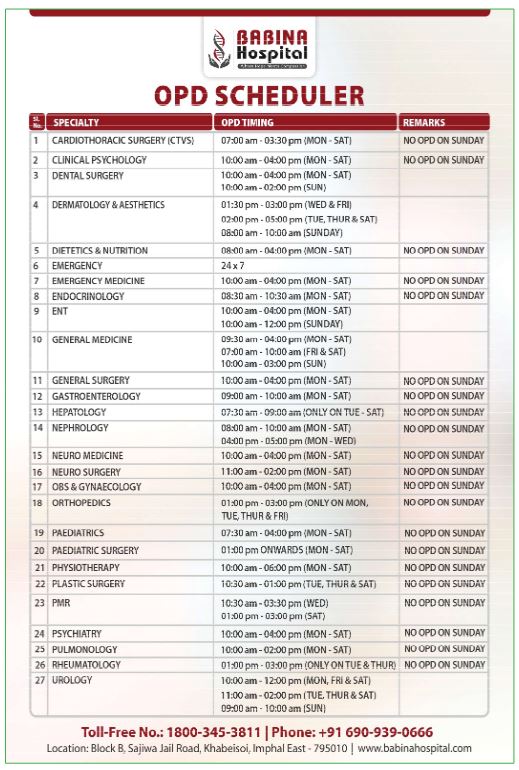
An estimated 10.5 percent of medicines worldwide are substandard or falsified, according to the World Health Organization (WHO). A much higher prevalence – around 40 percent – is reported for Africa. A new detection test developed by UK researchers might help weed out poor-quality medicines before they cause harm.
Substandard medicines result from poor manufacturing and quality-control practices as well as inadequate storage conditions, whereas falsified medicines are produced and labelled with the intent to defraud the consumer. Both kinds of poor-quality medicine claim to be something they are not. They are often indistinguishable from the genuine products, making them difficult to spot without running detection tests on their contents.
Poor regulatory controls or weak pharmaceutical governance allow these poor-quality pharmaceuticals to reach the market. And that can happen anywhere. Studies in the UK and Canada show substandard medicines, with reported issues of contamination and stability, are a greater problem in these countries than falsified medicines. In March 2022, in the UK, pharmaceutical manufacturer Pfizer recalled its blood-pressure medicine Accuretic because substandard batches were found containing a higher-than-acceptable amount of nitrosamine. Nitrosamine is a harmful impurity that can cause cancer if it is taken in high enough quantities over a prolonged period. This recall drew some local media attention, as did Pfizer’s recall of another blood-pressure medicine distributed outside the UK just six weeks later.
In this case the medicine was recalled before it reached consumers, so the tone of the media coverage was that this was a minor issue, easily addressed by the regulatory process. But if regulation fails and a poor-quality medicine is ingested, the consequences can be severe.
Substandard medicines with too little of the stated active pharmaceutical ingredient encourage the rise of antimicrobial-drug-resistant infectious diseases such as malaria, HIV and tuberculosis. The small amount of active ingredient is enough for the medicines to pass standard screening tests, but the dosages are too low to be effective – which can be deadly.
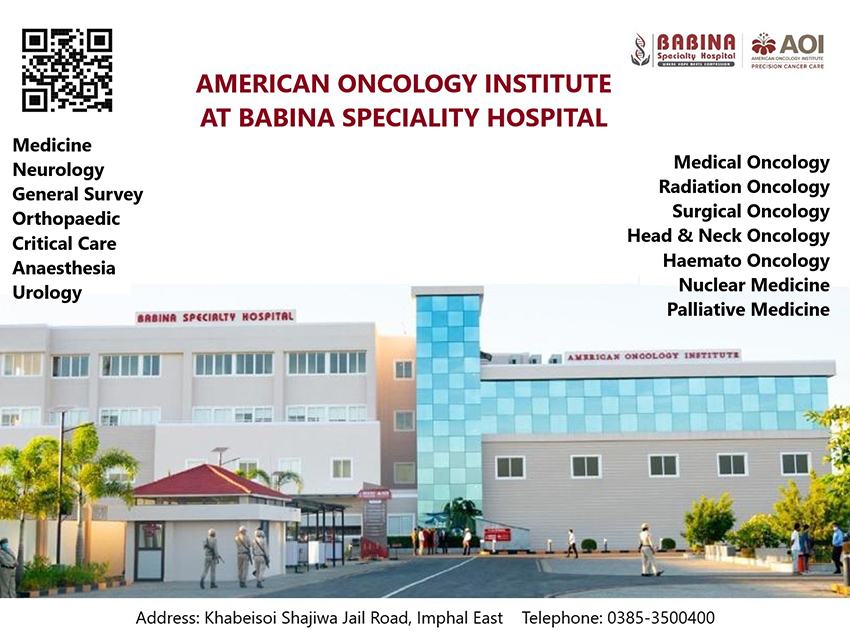
Substandard or falsified antimalarials cause an estimated 120,000 deaths from malaria each year in Africa alone, the WHO reports. Worldwide, substandard and falsified antimalarials are responsible for the deaths of over 150,000 children annually, according to a 2019 report by the American Journal of Tropical Medicine. Generic and branded medicines for infectious diseases as well as for chronic illnesses such as heart disease, diabetes and cancer have become prime candidates for poor-quality medicines. Antimalarials and antibiotics are among the most commonly reported substandard and falsified medical products, especially in Africa, because of the huge burden of infectious diseases across the continent. High-demand over-the-counter medicines containing paracetamol, for mild pain relief and to reduce fever, have also been reported as substandard or falsified. In recent years, expensive biotechnology-derived drugs, including vaccines, have been prone to falsification. There is mounting evidence that the COVID-19 pandemic has accelerated the problem of counterfeit medicines. The pandemic created increased demand for illegally produced medicines as the public turned to unregulated websites to purchase reputed treatments. Meanwhile, national lockdowns disrupted supply chains and testing protocols, making it harder for poor-quality medicines to be detected. A growing volume of falsified medicines associated with the novel coronavirus – for example, chloroquine – has been on sale, especially in regions such as Africa. Illegally imported antivirals have appeared in the UK, and fake COVID vaccines have been sold in Africa, China, India, Mexico and Poland. Interpol noted an 18-per-cent rise in the amount of counterfeit antiviral medicines it seized in 2020 compared to its corresponding operation in 2018. In the UK, Brexit has exacerbated this public health problem. The Royal Pharmaceutical Society worries the UK is no longer protected by the Falsified Medicines Directive (FMD), Europe’s anti-counterfeit medicines legislation. The UK’s medicines regulatory agency has identified an alarming 15,000 counterfeit medicines in the UK supply chain since the UK left the European Union in January 2020. To help shield consumers from substandard and falsified medicines, UK researchers are investigating simpler and faster ways of detecting them. They have developed a method of using a portable spectroscopy device to screen a pharmaceutical sample. The screening test involves direct analysis of the pharmaceutical sample or uses a small amount of powdered sample. This yields a chemical fingerprint unique to a medication, and shows the amount of the active pharmaceutical ingredient in that sample. This screening test takes a few seconds and can be performed by staff with limited training. Conventional surveillance methods are expensive, take longer to analyse a medicine, and require well-equipped laboratories and staff with expertise in the area – all major obstacles for low-resource countries. The need for and value of this research was demonstrated by the researchers’ collaborations with Kenya’s medicines regulatory body, where the analytical methods developed were applied to a real-world setting and the results were compared with conventional surveillance methods.
It makes no difference to a patient whether a medicine is substandard or falsified because the impact on their health is the same. The most important thing is being able to tell whether a medicine is what it claims to be.
Regulatory and technological measures are needed globally to tackle the substandard and falsified medicines pandemic. Greater public awareness of this growing healthcare issue is also needed. In the meantime, a new, simple detection test can help stop poor-quality products from reaching consumers who only seek to take their medicines in good faith.
Professor Sangeeta Tanna is Professor of Pharmaceutical Analysis at the Leicester School of Pharmacy in the Faculty of Health and Life Sciences at De Montfort University. Her research interests include the rapid identification of substandard and falsified medicines using spectroscopic and ambient ionisation mass spectrometry techniques. Dr Rachel Armitage is a Senior Laboratory Technician at the Leicester School of Pharmacy in the Faculty of Health and Life Sciences at De Montfort University. She has a PhD focusing on the rapid detection of substandard and falsified medicines. The authors have declared no conflict of interest in relation to this article. Image by Jack Sem, published under Creative Commons.
Originally published under Creative Commons by 360info™.